Tip of the Iceberg
Submitted by:
Annie Massart, MD
Assistant Professor
Hospital Medicine
Department of Medicine
STORY AND CASE:
A 49-year-old woman with history of multiple meningiomas (s/p multiple resections complicated by intracranial abscess requiring bifrontal craniectomy for drainage with subsequent bifrontal prosthetic cranioplasty), prior stroke with mild residual left-side weakness, and ventriculoperitoneal shunt placement for pseudomeningocele presented to the emergency department (ED) with one day of redness and swelling near her left medial eyebrow. She first noticed the redness and swelling on the morning of admission. There was no recent trauma to this area. There was mild pain over her eyebrow, but no headache, fevers, or chills.
On presentation, she was afebrile. Her heart rate was 116 and the rest of her vital signs were normal. Just superior to her left medial eyebrow, she had a nickel-sized area of erythema and tenderness. There was no induration or swelling. Her neurologic exam was notable only for mild weakness on her left which was unchanged from her baseline. Labs were significant for white blood cell count of 15.9 k/mcL with 78% neutrophils and a c-reactive protein (CRP) of 110.3 mg/L.
A head computerized tomography (CT) scan was obtained which was concerning for obstructive hydrocephalus. Neurosurgery was consulted and they believed the changes noted were chronic, related to her multiple prior surgeries and known diffuse meningiomas. She was admitted to medicine for treatment for facial cellulitis. She had a severe allergy to cephalosporins and so was started on clindamycin.
The subsequent morning, she experienced worsening of her facial pain. Physical exam demonstrated a new marked protuberance over her left medial eyebrow with fluctuance present. Edema had developed and was tracking dependently into both her left and right eyelids. The rest of her exam was unchanged, and she denied new symptoms. Repeat labs were notable for worsening leukocytosis to 16.3 k/mcL.
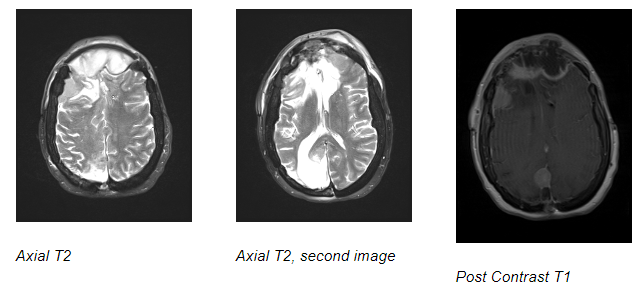
To address this new swelling, Ear, Nose, and Throat (ENT) and neurosurgery were consulted. She subsequently underwent a magnetic resonance imaging (MRI) of her brain with and without contrast to further evaluate it.
What’s the diagnosis?
ANSWER AND EXPLANATION
Her MRI brain revealed a large peripherally enhancing and centrally diffusion-restricting extra-axial collection subjacent to the entire bifrontal cranioplasty ~2.9 x 6.9 x 5.6 cm, volume ~56 cc consistent with a large extra-axial abscess. There was mass effect on the underlying brain parenchyma. Signal abnormality involving the left aspect of the cranioplasty suggested infected hardware, with contiguous extension of infection into the forehead soft tissues with additional soft tissue abscess and extensive facial cellulitis. This soft tissue extension of her intracranial abscess through the cranioplasty was the source for the new fluctuance noted on exam.
Her antibiotics were changed to vancomycin and meropenem, and she was taken to the operating room for surgical drainage. Upon removal of the cranioplasty, a large lake of pus was found and was evacuated. Operative cultures remained negative, potentially related to preoperative antibiotics. She recovered well in the neuro-intensive care unit (ICU). ENT performed bedside flexible fiberoptic laryngoscopy to evaluate for a possible sinus etiology of her infection but there was none noted. She had a peripherally inserted central catheter (PICC) line placed and was discharged home 6 days post-surgery with plans to complete a 4-week course of IV meropenem.
FINAL DIAGNOSIS
Intracranial epidural abscess
DISCUSSION
Intracranial epidural abscess is an uncommon intracranial infection. In a case series of over 4,000 patients admitted for intracranial sepsis, only 1.6% had an intracranial epidural abscess. The most common symptoms at presentation included fever, neck stiffness, and periorbital edema. Compared to other forms of intracranial abscess, patients are generally less toxic appearing at the time of presentation. Paranasal sinusitis is the most common etiology, but cranioplasty is known to be a potential source. Although it most commonly develops in the months following surgery, there are case reports of infections developing 20 years after surgery. Although MRI imaging is more sensitive, epidural abscesses are often visualized on CT imaging (though CT is less sensitive early in the course).
Intracranial abscess was not suspected on admission due to our patient’s lack of fever, headache, time since surgery, and lack of acute findings on her CT head. This may be related to decreased sensitivity of head CT in the setting of her multiple baseline intracranial abnormalities including meningiomas and frontal lobe encephalomalacia. This case highlights the importance of having a low threshold to pursue MRI imaging when patients demonstrate evidence of a soft-tissue infection overlying a cranioplasty. Patients may be well-appearing despite harboring a potentially life-threatening infection.
REFERENCES
Nathoo, Narendra F.C.S.; Nadvi, Syed Sameer F.C.S.; van Dellen, James Rikus Ph.D. Cranial Extradural Empyema in the Era of Computed Tomography: A Review of 82 Cases. Neurosurgery 44(4):p 748-753, April 1999.
Coyne TJ, Kemp RJ. Intracranial epidural abscess: a report of three cases. Aust N Z J Surg. 1993 Feb;63(2):154-7. doi: 10.1111/j.1445-2197.1993.tb00068.x. PMID: 8297308.
Gürbüz MS, Celik O, Berkman MZ. Infection of cranioplasty seen twenty years later. J Korean Neurosurg Soc. 2012 Nov;52(5):498-500. doi: 10.3340/jkns.2012.52.5.498. Epub 2012 Nov 30. PMID: 23323175; PMCID: PMC3539089.


Be the first to comment on "Faculty Development Case of the Month: February 2023"