Emory Division of Digestive Diseases Monthly Clinical Vignette Conference
Submitted by:
Manjusha Das, MD
Assistant Professor
Division of Digestive Diseases
Department of Medicine
Emory University School of Medicine
CASE
A 41-year-old African American female presented to GI clinic for follow up regarding her liver disease. She was a known patient to the GI clinic and was being followed for a diagnosis of primary sclerosing cholangitis (PSC). She initially presented in 2015 with elevated bilirubin and concern for choledocholithiasis and underwent endoscopic retrograde cholangiopancreatography (ECRP) which noted stones as well as stricturing concerning for possible PSC. Stone removal and biliary stent placement were performed and she followed up with GI at Grady Memorial Hospital. Repeat ERCP noted previously placed biliary stents as well as cholangiographic findings consistent with PSC. She subsequently underwent colonoscopy for evaluation of underlying inflammatory bowel disease; however, no endoscopic or histologic disease was noted.
Past medical history was notable of Hirschsprung disease with a prior colonic resection with entero-colonic anastomosis, during infancy. The patient denied any active alcohol use or other medication use to contribute to underlying liver disease. However, she was a former heavy drinker in 2010.
Surveillance MRI from July 2021 was negative for evidence of cirrhosis, hepatocellular carcinoma (HCC), any dominant strictures or progression of her PSC. By November 2021 she presented with severe vaginal bleeding and required hospitalization where she was noted to have severe coagulopathy and INR >10. Mixing study indicated factor deficiency, which was thought to be due to liver disease and was corrected with oral vitamin K. Subsequently, imaging noted a 7 cm left adnexal mass consistent with an endometrioma causing severe left hydronephrosis. Plans were being made for ureteral stent placement; however, her liver enzymes began to elevate as well as the INR, limiting and procedural interventions.
Due to the complexity of her history and concern for impending hepatic failure she was admitted to Grady for further inpatient workup.
Admission labs notable for:
| Total bilirubin | 9.5 mg/dL |
| Direct bilirubin | 5.9 mg/dL |
| AST | 149 |
| ALT | 134 |
| Alk Phos | 900 U/L |
| INR | 5.9 |
| Viral Hepatitis | negative |
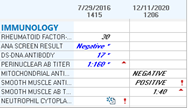
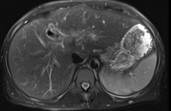
Autoimmune serologies and an image of admission MRI abdomen are shown below:
In patient ERCP was performed and no dominant stricture or filling defects were noted.
Liver biopsy was performed during hospitalization and final pathology noted: severe plasma cell infiltrates and severe lobulitis, along with focal fibrosis and ductopenia. There was no evidence of iron deposition or cirrhosis.
FINAL DIAGNOSIS?
Autoimmune Hepatitis/Overlap Syndrome
DISCUSSION
In hepatology, overlap syndrome is a clinical descriptor of various forms of autoimmune hepatobiliary disease, which includes features of autoimmune hepatitis (AIH), primary biliary cirrhosis (PBC) or primary sclerosing cholangitis (PSC). Autoimmune Hepatitis Overlap Syndrome is a rare syndrome mostly described in young adults2.
The diagnostic criteria are characterized by overt cholangiographic or histologic findings of typical PSC with robust histologic features of AIH. Thus, liver biopsy is necessary for diagnosis which was the case for this patient. Perinuclear antineutrophil cytoplasmic antibody (p-ANCA), ANA, and smooth muscle antibody (SMA) are frequently positive. Histologic features of interface hepatitis are pathognomonic for AIH.
In overlap syndrome, immunosuppression therapy is similar to that used to AIH. Prednisone of 40-60 mg/day is standard starting dose and Azathioprine is added as steroid-sparing agent later on once transaminases begin to improve1. Specifically, for PSC-AIH overlap the addition of ursodeoxycholic acid (UDCA) may be beneficial, although it is still unclear if this improves morbidity or mortality.
CITATIONS
- Kerkar N MD, Autoimmune Hepatitis, Sclerosing Cholangitis, and Autoimmune Sclerosing CHolangisis or Overlap Syndrome. Clinical Liver Disease 2022.
- Bunchorntavakul C MD, Diagnosis and Management of Overlap Syndromes. Clinics in Liver Diseaes. 2015.


Be the first to comment on "Faculty Development Case of the Month: June 2022"