Clinical Cases from Emory Division of Hospital Medicine Annual Clinical Vignette Conference
“The matters of story and size”
Submitted by:
Kyle James, MD
Assistant Professor of Medicine & Senior Physician
Division of Hospital Medicine
Emory Department of Medicine
Maaz Ahmed, MD
J. Willis Hurst Internal Medicine Residency Program
Emory Department of Medicine
Tyler Kristoff, MD
J. Willis Hurst Internal Medicine Residency Program
Emory Department of Medicine
Edited by Yelena Burklin, MD, FHM, FACP
CASE
A previously healthy 35-year-old woman presented with an acute onset of fever 38.3° C, progressive dizziness, and fatigue that started 24 hours before presenting to the hospital. Three weeks prior, she experienced back pain and difficulty upon taking deep inspiration that was treated with a 10-day course of levofloxacin. The pain subsided; however, frothy urine upon voiding developed. Additional history included a 30 lbs weight loss over the past four months and gingival bleeding following dental prophylaxis procedure. On admission, her vital signs included oral temperature 37.7° C, blood pressure 146/81 mmHg, heart rate 96 beats per minute, respiratory rate 18 breaths per minute, and oxygen saturation 98% on room air. Upon physical examination, lungs were clear to auscultation, and she had no costovertebral angle tenderness. The rest of the physical examination was reported normal. Laboratory evaluation revealed a white blood cell count of 4,4 x 103 /µL, hemoglobin of 7.9 gm/dL, hematocrit of 25.8%, and platelet count of 120 x 103 /µL. Blood urea nitrogen was 20 mg/dL, creatinine was 2.09 mg/dL, and alkaline phosphatase was 354 unit/L. Urinalysis revealed a random urine protein of 151 mg/dL and random urine creatinine of 292 mg/dL. Additional diagnostic investigations including blood cultures, chest X-ray, and urinalysis were unremarkable, with no evidence of an underlying infection.
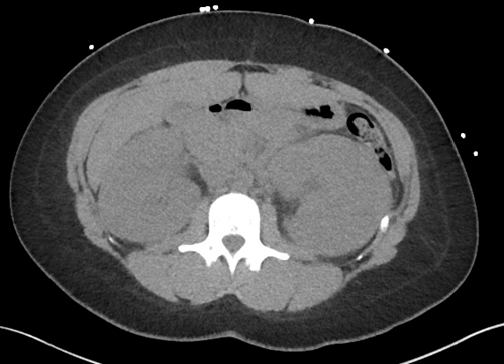
Computed tomography of the chest, abdomen, and pelvis was obtained, and the image of abdominal findings presented below:
Following the results of abdominal computed tomography, patient had serum protein electrophoresis performed, which revealed elevated free kappa light chains at 36 mg/L, prompting pursuit of a bone marrow biopsy. The results of the bone marrow biopsy revealed B-cell acute lymphoblastic leukemia.
What is your diagnosis?
FINAL DIAGNOSIS
Acute renal failure due to bilateral nephromegaly as a rare manifestation of B-cell acute lymphoblastic leukemia.
Hospitalization course
Fevers persisted for three days reaching a maximum temperature of 39.6° C. Additional laboratory studies, including HIV ELISA, Antinuclear antibodies, Anti-double stranded-DNA antibodies, C3 and C4 complement levels, and Anti-neutrophil cytoplasmic antibodies, were unremarkable. Alkaline phosphatase had a bimodal value distribution that resulted in transaminitis on hospital day five. After receiving the results of bone marrow biopsy, the patient was promptly started on daunorubicin, vincristine, and leuprolide chemotherapy which led to the resolution of nephropathy.
DISCUSSION
Bilateral nephromegaly is a rare finding that includes specific differential diagnoses. In the absence of obstructive uropathy, bilateral nephromegaly usually represents an underlying autoimmune disease or an infiltrative process. Common autoimmune diseases that should be included in the differential diagnosis are lupus, acute glomerular nephritis, acute interstitial nephritis, and renal vasculitis. The differential diagnosis for infiltrative processes includes amyloidosis, multiple myeloma, and hematologic malignancies. Other possible etiologies include sickle cell disease, thalassemia, and HIV nephropathy. In this case, the presence of type B symptoms was suspicious for malignancy, which in conjunction with elevated free kappa light chains, included a bone marrow biopsy for confirmatory diagnosis.
Association of bilateral nephromegaly and proteinuria should prompt clinicians to search for the underlying etiology, and diagnostic work-up must include considerations for autoimmune, infiltrative, and infectious processes. Close attention to the history and physical examination is necessary because further appropriate laboratory investigation will help narrow the differential and allow for a timely diagnosis.
CITATIONS
- Vijayasekharan K, Bhat K V, Venkatagiri AM, Godkhindi VM, Laxminarayana SLK, Belurkar S. Bilateral massive nephromegaly-A rare presentation of t-cell acute lymphoblastic leukemia. Leuk Res Rep. 2021;15:100246. Published 2021 May 19. doi:10.1016/j.lrr.2021.100246
- Tamura Y, Sumiyoshi R, Yamamoto T, et al. Bilateral nephromegaly due to direct leukemic cell invasion in the initial and relapse phases of T-cell acute lymphoblastic leukaemia: A case report. Medicine (Baltimore). 2021;100(51):e28391. doi:10.1097/MD.0000000000028391
- Kawano-Yamamoto C, Muroi K, Mori M, Nagai T, Ozawa K. Leuprorelin acetate for female patients with newly diagnosed acute leukemia receiving chemotherapy. Int J Hematol. 2007;86(2):199-201. doi:10.1532/IJH97.07051


Be the first to comment on "Faculty Development Case of the Month: March 2022"