Emory Division of Digestive Diseases Monthly Clinical Vignette Conference
“Not all colitis is the same”
Submitted by:
Manjusha Das, MD
Assistant Professor
Division of Digestive Diseases
Department of Medicine
Emory University School of Medicine
CASE
A 24-year-old female presented to the emergency room with complaints of worsening rectal bleeding. She has no known past medical history, and reports symptoms of abdominal pain, cramping, and urgency with defecation for the past several weeks. She has associated poor oral intake and unintentional weight loss of approximately 10 pounds. She had presented to an outside hospital a few weeks prior to presentation and was prescribed a course of Levaquin and Clindamycin. She reports her symptoms worsened after the antibiotics. She denies any outside travel, or sick contacts. She denies any alcohol use, smoking or any illicit drug use. Review of symptoms indicated bilateral knee pain and wrist pain.
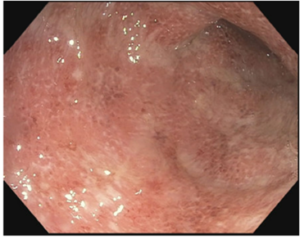
On presentation to our facility she was hemodynamically stable and afebrile. CBC noted a hgb of 9 g/dL and platelet count of 400 K/mcL. Her chemistry was notable for albumin of 2.5 g/dL and ESR of 40 mm/h CRP of 50 mg/L. She has diffuse abdominal tenderness, no guarding or rigidity on exam. She completes a CT abdomen in the emergency room which notes diffuse bowel wall thickening. She proceeds to have an inpatient colonoscopy, which notes severe colitis.
Endoscopic images from flexible sigmoidoscopy (severe colitis)
CT abdomen imaging (bowel wall thickening)
FINAL DIAGNOSIS?
Acute severe ulcerative colitis
DISCUSSION
Ulcerative colitis is a chronic inflammatory bowel disease with peak onset in early adulthood. This disease is naturally relapsing and remitting. 20% of these patients may require hospitalization for severe disease. Rates of colectomy in acute severe ulcerative colitis range from 25-30%.
Prognostic factors which help to predict the aggressiveness of disease and potential need for colectomy are: young age of diagnosis (<40 years), extensive disease, severity of endoscopic disease activity, presence of extra-intestinal manifestation, early need for corticosteroids, and elevated inflammatory markers.
It is important to rule out concomitant infectious etiologies specifically Clostridium Difficile. Severe disease is defined by Mayo clinic scores >6 and endoscopic severity scores of 2 or 3. Generally, patients with Hgb <10 g/dL, ESR of 30 mm/h, and albumin <3 g/dL indicate severe colitis. The patients risk deep ulcers which increase the risk of perforation or toxic colitis and need for emergent surgery. Remember despite their bleeding these patients are high risk for thromboembolism and should always receive DVT prophylaxis.
This patient responded well to prednisone therapy. Per guidelines doses of methylprednisolone of 40-60 mg/d is sufficient to treat acute severe UC.
CITATIONS
- Feuerstien J. et al. AGA clinical practice guidelines on the management of moderate to severe ulcerative colitis. Gastroenterology 2020.
- Rubin D. et al. ACG Clinical Guideline: Ulcerative Colitis in Adults. American Journal of Gastroenterology 2019.




Be the first to comment on "Faculty Development Case of the Month: April 2022"