Please view the August 2021 Case of the Month below:
Submitted by:
TaRessa Wills, MD, FACP
Assistant Professor of Medicine
Division of Hospital Medicine
Emory University School of Medicine
Grady Memorial Hospital
Edited by: Manpreet S. Malik, MBBS, FHM
STORY AND CASE
36-year-old female presented to the Emergency Department (ED) with a 3-day history of dyspnea, nausea, vomiting, abdominal pain and distention. She reported that about 4 years prior to this admission, she developed cyclic pain and symptomatic recurrent ascites while living in Cincinnati. Prolonged work up was done without identifying etiology. Eventually she had a diagnostic laparoscopy and was told she had endometriosis although peritoneal implants were not seen. She reported variation in abdominal distension and pain with her menstrual cycle. About a year prior to this presentation, she required a large volume paracentesis for ascites. She was started on Lupron with improvement of symptoms. However, 6 months after therapy, she was told she needed a new doctor because she was a “medical mystery”. She was on no menstrual suppression after this. With a new provider she was started on Orilissa (elagolix) and Aygestin (norethindrone) 2 months prior to presentation. Patient had no history of alcohol or drug use.
On exam, vital signs were normal. Abdominal exam showed distended abdomen with mild diffuse tenderness and no rebound.
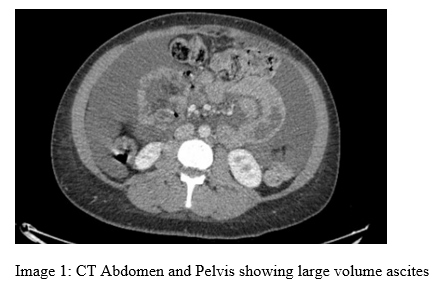
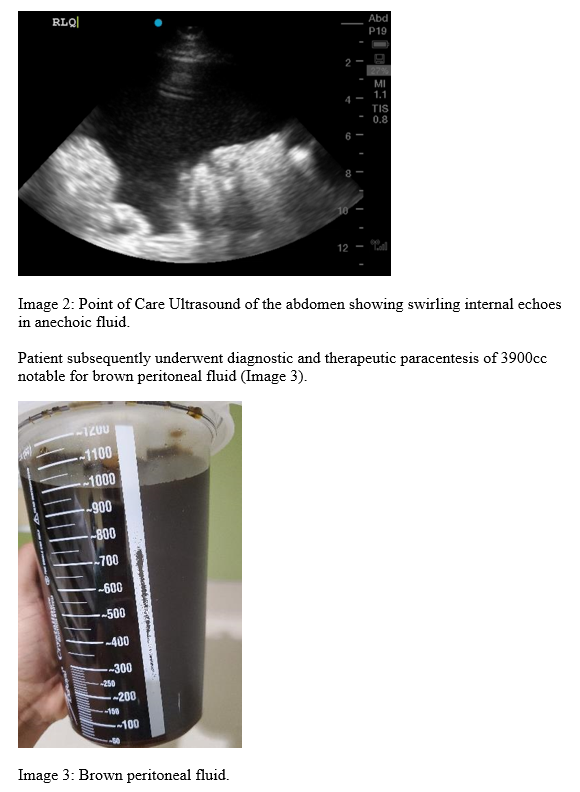
Work up in the ED, included a CT scan of her abdomen and pelvis, and noted large volume ascites (Image 1). Bedside ultrasound showed large volume ascites as well with shimmering echogenic dots in otherwise anechoic fluid (Plankton sign, Image 2).
Fluid analysis with WBC 63 units/mcL, RBC 26,516 units/mcL, and cytology was consistent with CD68 positive hemosiderin laden macrophages. Patient had significant symptomatic improvement post procedure prompting discharge home with Gynecology follow up to further discuss management options of her endometriosis.
What is the diagnosis?
Hemorrhagic ascites (chocolate brown ascites) due to endometriosis with peritoneal involvement.
Discussion
Recurrent hemorrhagic ascites secondary to endometriosis is an extremely rare presentation. The first case of endometriosis-related ascites was described by Brew in 1954 with less than 100 cases reported since then. Based on systematic reviews, cases were seen in nulliparous women, with African American women making 63% cases in this review. 38.1% presented with pleural effusion. Abdominal distension, anorexia or weight loss, abdominal pain, and menometrorrhagia were the most common symptoms.
Ectopic sites for endometriosis diagnosed by laparoscopy include broad ligament, intestinal wall, uterus, ovary, peritoneum, and so on. The physiopathology of endometriosis-related ascites is not completely known. Predominant theories include peritoneal irritation from ruptured endometrial implants, subdiaphragmatic lymphatic obstruction, and retrograde menstruation. Anemia secondary to this condition is not a usual presentation and massive hemorrhage remains even more rare.
The long-term management of recurrent massive ascites caused by endometriosis is difficult. Medical therapy, including GnRH analogs, danazol, and progestogens, has been used with variable success. A literature review showed that endometriosis-related ascites have a high recurrence rate of >50% after unilateral oophorectomy or cystectomy but have no recurrence after bilateral salpingo-oophorectomy(BSO). Thus, patients who undergo conservative surgery or medical therapy should be closely followed up. Our patient was unwilling to undergo hysterectomy with BSO which had previously been recommended and therefore decided to follow up with gynecology to continue hormone therapy.
Acknowledgements: Dr. Malavika Kapuria, MD and Emory Obstetrics and Gynecology at Grady for assisting with the management for this patient.
Citations
- Wang, Xue BMeda; Li, Yiling MDa,∗; Tong, Jing MDa; Chang, Bing MDa; Zhang, Yi PhDb; Liu, Yanjun MDc; Bing, Hao BMeda; Guo, Liping BMeda; Li, Dan MMeda Endometriosis presenting with recurrent massive hemorrhagic ascites and diagnosed by core needle biopsy, Medicine: May 2019 – Volume 98 – Issue 19 – p e15477 doi: 10.1097/MD.0000000000015477
- Gungor T, Kanat-Pektas M, Ozat M, et al. A systemic review: endometriosis presenting with ascites. Arch Gynaecol Obstet 2011;283:513–8.
- Brew A. Endometriosis including endometriosis of the diaphragm and Meigs syndrome. Proc R Soc Med 1954;47:461.
- El-Newihi HM, Antaki JP, Rajan S, et al. Large bloody ascites in association with pelvic endometriosis: case report and literature review. Am J Gastroenterol 1995;90:632–4.
- Ussia A, Betsas G, Corona R, et al. Pathophysiology of cyclic hemorrhagic ascites and endometriosis. J Minim Invasive Gynecol 2008;15:677–81.


Be the first to comment on "Faculty Development Case of the Month: August 2021"