From the Division of Hopsital Medicine
“It’s not COVID…for once!”
Submitted by:
Melissa Youssef Beshay, MD
Assistant Professor of Medicine
Division of Hospital Medicine
Department of Medicine
Emory University School of Medicine
Edited by:
Lou Kerkhoff, MD
Division of Hospital Medicine
STORY AND CASE
While in training, during the pandemic, my attending told me that there are no Zebras, there is only COVID. Now as the pandemic is coming to an end, it appears that the Zebras may be returning as the following case illustrates.
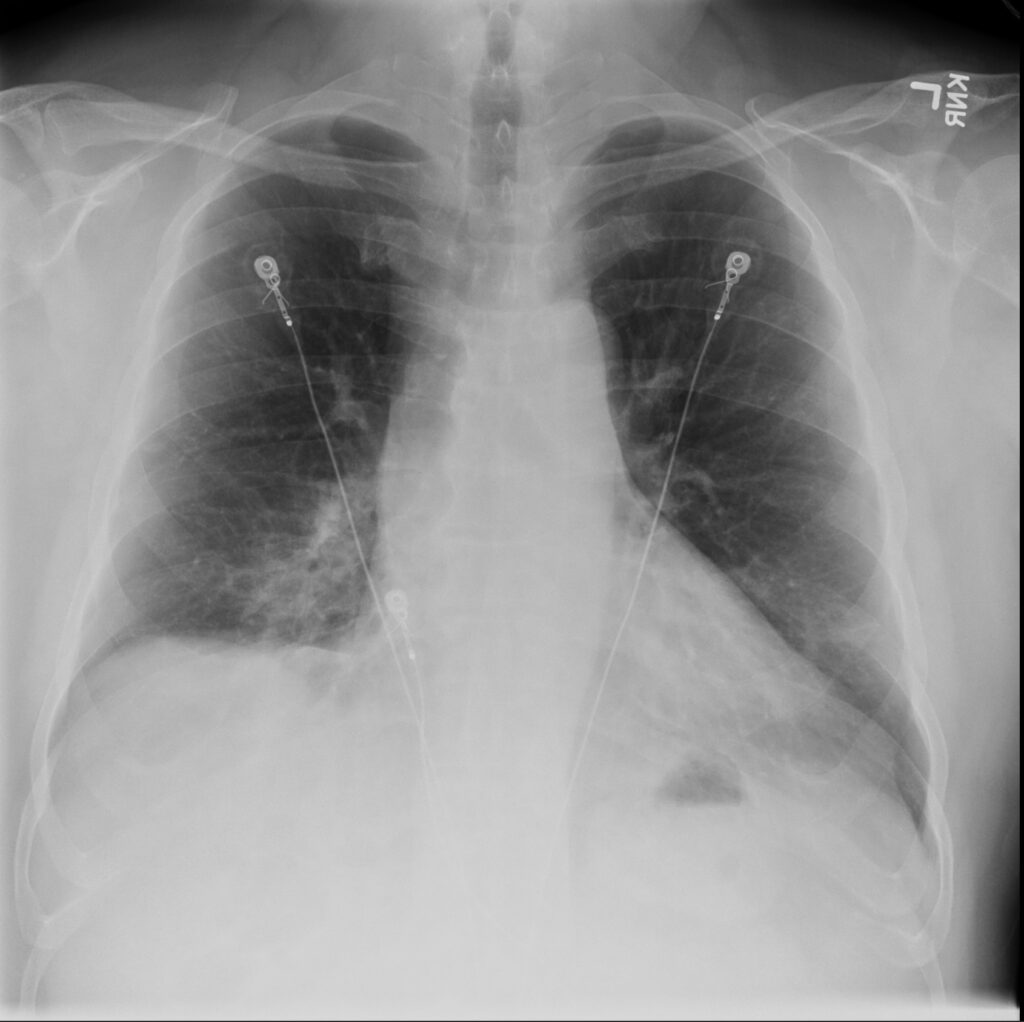
A 59-year-old Hispanic male presented to the emergency department (ED) with complaints of high fever, profuse watery diarrhea, and a dry cough. His symptoms began after attending a wedding in Mexico. He was careful to drink only bottled water, but he did eat some of the food there. His symptoms began with the fevers and then progressed to include diarrhea. The diarrhea began to improve, but the fevers continued, prompting him to come to the ED. He also noted that he had a mild cough, but it had only just started on the day he came to the ED. The ED physician ordered an abdominal CT that was unremarkable except for ground glass opacities in the lower lung fields. A chest x-ray showed a right lower opacity. The chest findings were puzzling because the patient’s chief complaints included diarrhea and high fever, but his cough was only minor. On exam, he was febrile at 39.6 C, heart rate was 121, blood pressure was 101/61, and he was saturating well on room air. His abdominal examination was benign, and he had crackles in all lung fields. Past medical history was significant for Immune-mediated necrotizing myositis (IMNM) on methotrexate and coronary artery disease (CAD) s/p myocardial infarction (MI) and stent—these conditions suggest that the patient was immunocompromised. The admitting hospitalist ordered a Chest CT which showed bilateral ground glass opacities. Admission labs were remarkable other than mild leukocytosis, low procalcitonin, negative respiratory viral panel and a NEGATIVE COVID test.
On admission, given diagnostic uncertainty and suspicion for a GI source of infection- he was started on piperacillin-tazobactam and linezolid. The Infectious Disease team was consulted and narrowed coverage to ceftriaxone and metronidazole—again with suspicion of GI source. A GI panel and stool studies were ordered, which were negative for Shiga toxin, Campylobacter, C difficile PCR and toxin. During the course of admission, the patient’s pulmonary symptoms worsened. A legionella urine antigen test was ordered and came back positive.
ANSWER AND DISCUSSION
The patient was diagnosed with Legionella pneumonia. He was then started on a 10-day course of levofloxacin.
According to the literature, Legionella pneumonia classically presents as a community-acquired pneumonia with mainly flu-like symptoms. The patient’s presentation of fever, cough and shortness of breath arising 5-10 days after travel, lobar infiltrates on CT, GI symptoms, and hyponatremia fit the classic presentation for legionella; however, the predominance of GI symptoms first was more concerning for GI infection and not necessarily pneumonia.
Legionella should be of high suspicion, however, as it occurs in outbreaks in association with water supplies in large facilities such as hotels, apartments or hospitals and is spread through the air conditioning system. The patient’s immunocompromised history also put him at high risk for disease. He also was made aware that several of the wedding attendees did get sick after the wedding with similar symptoms. Patients should be tested for Legionella if they have moderate to severe community-acquired pneumonia who require hospitalization, have a known exposure to Legionella (outbreak), or are immunocompromised. The Legionella urine antigen test has a sensitivity of 70-80% and specificity reaches 100% in patients with Legionnaires’ disease caused by L. pneumophila.
FINAL DIAGNOSIS
Legionnaires’ disease. serotype 1.
CITATIONS
- Fraser DW, Tsai TR, Orenstein W, et al. Legionnaires’ disease: description of an epidemic of pneumonia. N Engl J Med 1977; 297:1189.
- Sopena N, Sabrià-Leal M, Pedro-Botet ML, et al. Comparative study of the clinical presentation of Legionella pneumonia and other community-acquired pneumonias. Chest 1998; 113:1195.


Be the first to comment on "Faculty Development Case of the Month: July 2023"