Monthly Case from Emory Saint Joseph’s Hospital
When it’s not Pancreatitis … Don’t brush it off
Submitted by:
Maha Sulieman, MBBS
Assistant Professor
Division of Hospital Medicine
Department of Medicine
Co-written by:
Gayle Wong, MD and Reem Amhed, MD
Division of Hospital Medicine
Edited by:
Manpreet Malik, MD
Assistant Professor
Division of Hospital Medicine
CASE
The patient was a 72-year-old male with medical history of hypertension. He presented with fever and dull epigastric pain for 3 days. Physical exam was significant for epigastric and left periumbilical tenderness. He was febrile with a temperature of 38.4° F. Laboratory data revealed elevated white blood cells (18.0/μL), elevated inflammatory markers (ESR 39 mm/hr, CRP 134.80 mg/L), normal lipase of 27 unit/L, and a triglyceride level of 94 mg/dl. A CT scan of his abdomen and pelvis with intravenous (IV) contrast showed peripancreatic fat stranding around the head and uncinate process of the pancreas, suggesting acute pancreatitis, and inflammatory stranding adjacent to the third part of the duodenum, which was thought to be related to the pancreatic process. Gallbladder appeared normal on abdominal ultrasound and hepatobiliary scan. He was started on conservative management with bowel rest, IV fluid and pain medications.
The patient’s normal lipase level, lack of risk factors for pancreatitis including alcohol consumption, and absence of gallstones prompted the evaluation for another etiology of his pain. Esophagogastroduodenoscopy was pursued next and showed erythematous mucosa in the gastric antrum. MRI of the abdomen with was then performed and showed a perforating duodenal foreign body (possibly a fishbone) with transmural extension into adjacent mesentery, causing marked focal duodenitis and a peri-duodenal phlegmon. There was no evidence of pancreatitis on MRI.
FINAL DIAGNOSIS?
Small Bowel Perforation Caused By Ingestion of a Grill Brush Bristle
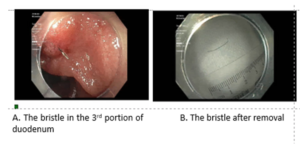
The MRI findings shifted the therapeutic focus from conservative to interventional management. Small bowel enteroscopy was performed and revealed a foreign body in the third portion of the duodenum that was successfully removed with snare. Upon close inspection, the foreign body was identified as a steel bristle from a grill brush. The patient recalled ingestion of grilled food prior to symptoms development. The patient required extended antibiotic therapy and close follow-up after discharge, and eventually recovered completely.
DISCUSSION
In the adult population, perforation of the small bowel caused by wire bristle ingestion appears to be a relatively common injury, likely due to the bristle’s small diameter and frequent angulation within the small bowel, though it is observed less frequently than oral or oropharyngeal injury.(1) Delays in diagnosis and removal of foreign bodies in the gastrointestinal tract can cause significant morbidity and mortality; consequences include perforation, bleeding, and abscess formation.
Depending on the site of penetration, clinical presentation may mimic more common medical conditions, e.g., gastritis if the bristle lodges in the stomach, or pancreatitis if the bristle is in the pancreas or duodenum. Micro-perforations of the small bowel are usually subtle and subacute in nature, and present with less severe symptoms than perforation in other parts of the gastrointestinal tract. Because management of common mimic conditions is mostly conservative, high clinical suspicion is necessary when clinical data is not consistent with the presumed diagnosis, as in our case.
CT scans are the preferred method of pre-procedural diagnosis and are recommended for initial localization and evaluation of complications, including bowel perforation.(2) Use of IV contrast enhances bowel wall layers and can obscure foreign objects. Non-contrast CT may be more sensitive in detecting the intrinsic contrast of the foreign body against nonenhanced bowel wall; however, this usually requires a pre-imaging high clinical suspicion of foreign body ingestion.(3)
MRI has excellent soft tissue resolution. Magnetic resonance cholangiopancreatography is particularly important in evaluation of the pancreas and biliary tract when initial images suggest a mimicker, like pancreatitis in our case. Despite higher cost and time needed for MRI, it is considered a less invasive localization method than endoscopic evaluation.(4) Multiple endoscopic versus surgical procedures maybe required for localization and safe removal.
CITATIONS
- Baugh TP, Hadley JB, Chang CW. Epidemiology of Wire-Bristle Grill Brush Injury in the United States, 2002-2014. Otolaryngol Head Neck Surg. 2016;154(4):645-9.
- Chen Q, Huang Y, Wu Y, Zhao K, Zhu B, He T, et al. A comparative study of small intestinal perforation secondary to foreign body and other non-traumatic causes. Ulus Travma Acil Cerrahi Derg. 2015;21(2):107-12.
- Kumar D, Venugopalan Nair A, Nepal P, Alotaibi TZ, Al-Heidous M, Blair Macdonald D. Abdominal CT manifestations in fish bone foreign body injuries: What the radiologist needs to know. Acta Radiol Open. 2021;10(7):20584601211026808.
- Olson MC, Navin PJ, Welle CL, Goenka AH. Small bowel radiology. Curr Opin Gastroenterol. 2021;37(3):267-74.


Be the first to comment on "Faculty Development Case of the Month: August 2022"