The Department of Medicine would like to congratulate our resident clinician innovators on their recent successful participation in the Georgia Tech/Emory Biomedical Engineering (BME) Capstone projects!
As part of the J. Willis Hurst Internal Medicine Residency Programs’ Distinction in Medical Innovation program, internal medicine residents successfully pitched relevant healthcare problems that were selected for medical device development by senior capstone BME teams this fall semester. Our residents served as key members of their teams, providing project leadership and key clinical guidance. The BME teams showcased their completed device solutions at the recent Georgia Tech Capstone Design Expo. This year, our residents pitched, developed and mentored five out of 32 BME teams.
Georgia Tech students highly value the opportunity to work with Emory faculty and residents as they receive credentialing and access for clinical observations at Emory Healthcare and Grady Health System facilities through the Student Training for Advancing Technologies Credentialing program (STAT), co-sponsored by the dean’s office at Emory’s School of Medicine. This program has afforded the Georgia Tech students critical opportunities to understand the need and the environments in which their innovations will be implemented.
View our residents’ projects and videos below:
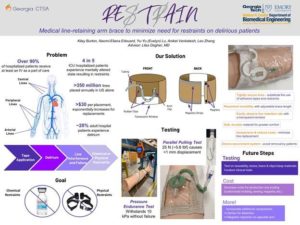
Lilas Dagher, MD (clinical mentor/sponsor)
“REsTrAIN” BME team members:
- Niket Venkatesh, Johns Creek, GA
- Kiley Burton, Williamson, GA
- Leo Zhang, Atlanta, GA
- Naomi-Eliana Edouard, Brooklyn, NY
- Yu-Yu Lu, Atlanta, GA
Description:
REsTrAIN. Medical Line Retainers for Restraint Prevention. Our product will provide Inpatient healthcare providers with a method to prevent patients from removing or interfering with invasive lines without the use of physical and chemical restraints.
Video presentation:
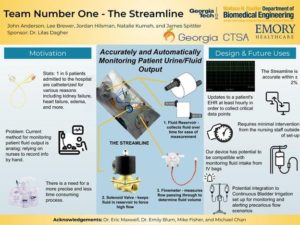
Lilas Dagher, MD (clinical mentor/sponsor)
“Team Number One” BME team members:
- James Spittler, Winter Garden, FL
- John Anderson, Clinton, NJ
- Jordan Hilsman, Rutledge, GA
- Lee Brewer, Oxford, GA
- Natalie Kumeh, Buford, GA
Description:
The Streamline. Automatic Urine Flow Monitor. A device for automatically monitoring the volume of a patient’s urine output so that doctors can make better informed treatment decisions, especially for patients in more critical conditions. The automatic nature of this device will reduce the need for nurses to manually check the urine volume present in urine collection bags and other receptacles.
Video presentation:
Lucie Calderon, MD and Adam Spandorfer, MD (clinical mentor/sponsor)
“Loco Moco” BME team members:
- Hajime Minoguchi, Cincinnati, OH
- Jeongjin Lee, Seoul, South Korea
- Seul Lee, South Korea
- Siyeon Park, Seoul, South Korea
- William York, Atlanta, GA
Description:
Loco Moco. Locomotive Video Capsule Endoscopy. Video Capsule Endoscopy is a process on the forefront of modern medicine in which a patient swallows an electronic capsule with cameras, LEDs, and bluetooth. It has been demonstrated to be the most effective method for diagnosing issues inside of the small intestine that are normally unidentifiable. However, patients with dysmotility problems have issues with digestion and moving food along their intestinal tract are not able to use this device due to the high risk of capsule retention. We have redesigned the device to reduce the risk of capsule retention for patients that have dysmotility issues.
Video presentation:
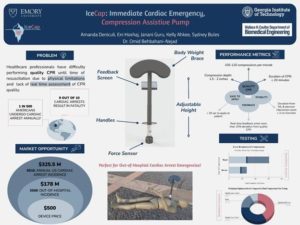
Omid Behbahani-Nejad, MD (clinical mentor/sponsor)
“IceCap” BME team members:
- Amanda Deniculi, Sao Paolo, Brazil
- Eni Hoxhaj, Korçë, Albania
- Janani Guru, Suwanee, GA
- Kelly Ahkee, West Palm Beach, FL
- Sydney Bules, West Chester, PA
Description:
IceCAP. CPR Assistive Device. Cardiopulmonary resuscitation (CPR) is the first and most important line of response for treating cardiac arrest. Our device addresses the difficulty healthcare professionals face while performing quality CPR by helping to mitigate physical limitations and providing real time assessment of CPR quality.
Video presentation:
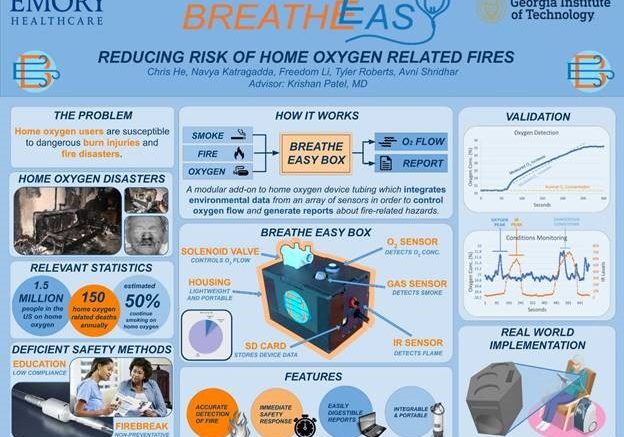
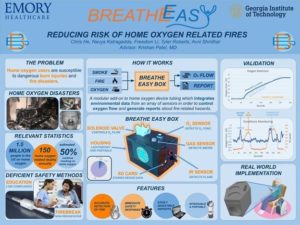
Krishan Patel, MD (clinical mentor/sponsor)
“Breathe Easy” BME team members:
- Avni Shridhar, Metairie, LA
- Christopher He, Marietta, GA
- Navya Katragadda, Smyrna, GA
- Tyler Roberts, Statesboro, GA
- Yunong Li, Guiyang, China
Description:
Breath Easy. Preventing burns from home oxygen therapy. Home oxygen therapy is commonly prescribed in the United States to treat pulmonary illnesses. Many patients use oxygen tanks and concentrators to provide consistent low-flow oxygen delivery, but these devices pose a risk of injury. Smoking, cooking, and other improper exposure to flames can cause life-threatening injuries which can be prevented by implementing a device to ensure patient safety. Current oxygen therapy devices on the market do not include safety mechanisms to prevent fire threats, putting users at high levels of risk. The Breathe Easy Box works by utilizing multiple transducers to collect data on the patient’s environment and controlling a valve to shut off oxygen flow if the risk of fire is present. The device is housed in a compact apparatus that can be attached to any existing oxygen therapy device. The sensor data is available as a centralized database to both physicians and the medical device companies which own the home oxygen devices, which can be used to better understand the patient’s environment. By implementing a preemptive response, the patient can continue to use their necessary oxygen therapy with decreased risk of life-altering injuries, medical costs, and property damage.
Video presentation:
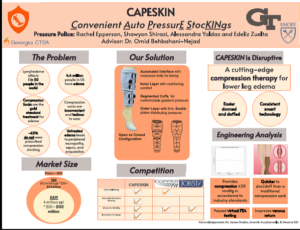
Omid Behbahani-Nejad, MD (clinical mentor/sponsor)
“Pressure Police” BME team members:
- Alessandra Yoldas, Fort Lauderdale, FL
- Edeliz Zuleta, Grovetown, GA
- Rachel Epperson, Friendswood, TX
- Shawyon Shirazi, Atlanta, GA
Description:
CAPESKIN. Convenient Auto PressurE StocKINgs. Patients have difficulty putting on their compression stockings, which decreases their compliance despite physician recommendations, leading to consequences such as lower extremity (read: leg) edema, development on varicose veins, serving as a nidus for infections and complications such as cellulitis, and even sepsis / amputation / death in extreme cases. Compression stockings come in various shapes and forms, and the general consensus is that by increasing the external pressure on the lower extremities of a patient, one increases the venous blood return in the fight against gravity back into the right side of the heart, the central pump of the human body. The issue lies in patients having difficulty with choosing which stockings to purchase, some requiring tailoring to fit their specific anatomy, along with other factors that make the process confusing for patients who just want a simple convenient “one-size-fits-all” solution to their chronic medical problem.


Be the first to comment on "Department of Medicine residents collaborate with biomedical engineering students on Georgia Tech/Emory Biomedical Engineering (BME) Senior Capstone projects"