Please view the June 2021 Case of the Month below:
Submitted by:
Jason Williams, MD
Assistant Professor, Division of Hospital Medicine
Emory Department of Medicine
“Refractory Hypoxia or Malfunctioning Pulse Ox?”
STORY AND CASE
76-year-old male with a past medical history of heart failure with preserved ejection fraction, coronary artery disease, and hypothyroid, taking dapsone and prednisone for bullous pemphigoid who presented with left upper extremity pain and swelling. The pain and swelling occurred after moderate trauma to the medial left bicep. An ultrasound confirmed the presence of a provoked DVT in the left upper extremity and he was started on a direct oral anticoagulant. In the emergency department his O2 saturation was 88% on 4 liters of nasal cannula oxygen. He was admitted for further work up of his hypoxia.
On review of systems, the patient noted that he had progressive shortness of breath for six months. He denied fever, chills, chest pain, cough, hemoptysis, orthopnea, and paroxysmal nocturnal dyspnea. His cardiopulmonary exam was normal.
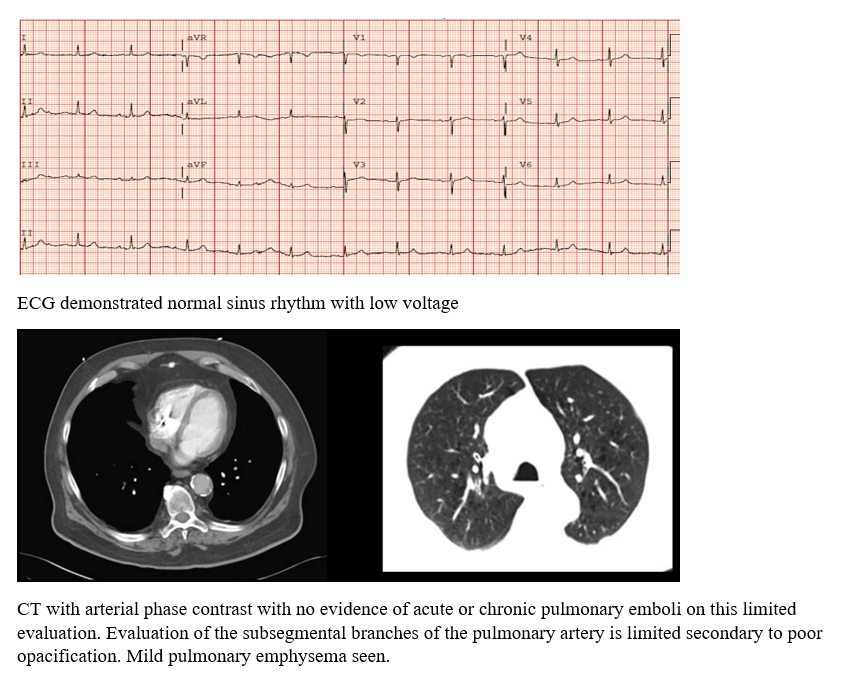
He had a normal WBC, hemoglobin, CRP, lactate, creatinine, BNP, and troponin. An ECG and CTA were obtained in the ED and the results are below. A bedside point-of-care ultrasound exam noted a normal central venous pressure of 3mmHg, normal ejection fraction, no pericardial effusion, and no signs of right ventricular dysfunction.
In the hospital his pulse oximetry was recorded at 87% on room air, and would only correct to 89% on 6 liters of oxygen. The wave form on the pulse oximetry was noted to be high quality. An aterial blood gas sample obtained on room air reported a PaO2 of 86mmHg (normal > 80), O2 saturation of 94%, normal A-a gradient, and normal PCO2.
What additional diagnostic test should be performed?
ANSWER AND EXPLANATION
FINAL DIAGNOSIS?
Test: Methemoglobin level of 9.8% (normal range < 2%). The patient was diagnosed with iatrogenic methemoglobinemia due to dapsone therapy.
DISCUSSION
When cyanotic patients do not improve with supplemental oxygen, clinicians should consider a right-to-left shunt or methemoglobinemia. Methemoglobin occurs when iron gets oxidized from Fe2+ to Fe3+ resulting in a conformational change in hemoglobin. As a result, the hemoglobin can no longer bind oxygen which markedly decreases tissue oxygen delivery. Methemoglobin also absorbs light at a different wavelength than the pulse oximeter resulting in an erroneous oxygen saturation around 85% regardless of the true hemoglobin oxygen saturation. The oxygen saturation of the arterial blood gas is also erroneous because this value is calculated based on the measured PaO2 which assumes normal oxyhemoglobin disassociation curve. Most blood gas analyzers can be programmed to specifically measure methemoglobin level if the lab is notified ahead of time.
Common symptoms of methemoglobinemia include cyanosis, shortness of breath, and brown coloration of the blood. The severity of symptoms increases with increasing levels of methemoglobin. Levels > 10% usually require treatment with methylene blue. Dapsone is responsible for about 42% of the cases of acquired methemoglobinemia.
This patient’s dapsone was stopped, he was given supplemental oxygen observed for 48 hours. Since his methemoglobin level was < 10% and his symptoms were mild, he was not given methylene blue. After 48 hours of observation, his methemoglobin level dropped to 7.2% and he was discharged home. Three months later his shortness of breath has completely resolved after stopping his Dapsone.
CITATIONS
- McMullen SM, Patrick W. Cyanosis. Am J Med. 2013 Mar;126(3):210-2. doi: 10.1016/j.amjmed.2012.11.004. PMID: 23410559.
- Cortazzo JA, Lichtman AD. Methemoglobinemia: a review and recommendations for management. J Cardiothorac Vasc Anesth. 2014 Aug;28(4):1043-7. doi: 10.1053/j.jvca.2013.02.005. Epub 2013 Aug 13. PMID: 23953868.
- Ash-Bernal R, Wise R, Wright SM. Acquired methemoglobinemia: a retrospective series of 138 cases at 2 teaching hospitals. Medicine (Baltimore). 2004 Sep;83(5):265-273. doi: 10.1097/01.md.0000141096.00377.3f. PMID: 15342970.
Acknowledgements:
- Amy Miller, MD, Assistant Professor, Division of Hospital Medicine, Atlanta VA Medical Center
- Erin Kim, MD, Assistant Professor, Division of Hospital Medicine, Atlanta VA Medical Center


Be the first to comment on "Faculty Development Case of the Month: June 2021"