Please view the March 2021 Case of the Month below:
Submitted by:
Erica Han, MD
Assistant Professor & Senior Clinician
Department of Medicine (Division of Hospital Medicine)
Emory University School of Medicine
Edited by Yelena Burklin, MD, FHM, FACP
“Not ‘nother pneumonia”
STORY AND CASE
A 35-year-old Black woman with history of alcohol and tobacco abuse presented to the hospital with progressive dyspnea and nonproductive cough for one month not responding to appropriate outpatient antibiotics (a course of azithromycin followed by levofloxacin) that were prescribed upon previous outpatient presentations. Six months prior to the current presentation, she was hospitalized for acute pancreatitis that was attributed to her alcohol binge drinking.
Upon arrival, patient denied any fevers, orthopnea, edema, or unintentional weight fluctuations.
Her admission vital signs revealed: T 36.8C, BP 135/85, HR 98, and SpO2 95% on ambient air. She was in mild respiratory distress after sitting upright in the hospital bed. She had no signs of volume overload as was evident by non-elevated jugular venous pressure and absence of peripheral edema. Her pulmonary exam was notable for mild expiratory wheezing. Laboratory findings were also unremarkable and in particular, her white blood cell count was within normal limits. Sputum and blood cultures were obtained, and respiratory viral panel along with an HIV ELISA test all returned negative.
She was started on intravenous vancomycin and piperacillin-tazobactam therapy, had been administered steroids and bronchodilators, however there was no clinical improvement.
Blood cultures and sputum cultures remained sterile.
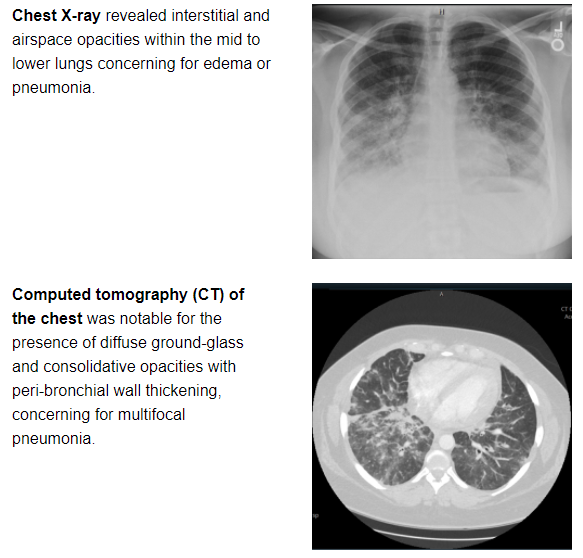
The images and the reported results of her chest X-ray and chest computed tomography are provided below:
Given low suspicion for an infectious process, patient was referred for an inpatient lung biopsy.
Inflammatory pneumonitis and interstitial lung disease, for which differential diagnosis is broad, were considered in the differential diagnosis. Pneumonitis or secondary organizing pneumonia could be due to undiagnosed connective tissue disease, vasculitis, respiratory bronchiolitis, sarcoidosis, or idiopathic etiology. Antinuclear antibodies (ANA), rheumatoid factor (RF), antineutrophil cytoplasmic antibodies (ANCA) were negative, and complements C3 and C4 returned normal.
Patient underwent video-assisted thoracoscopic (VATS) biopsy prior to hospital discharge.
What is your diagnosis?
FINAL DIAGNOSIS: Stage IV pancreatic adenocarcinoma with pulmonary lymphangitic carcinomatosis
Disease trajectory of interest:
Patient underwent first cycle of chemotherapy treatment with leucovorin, fluorouracil, irinotecan, and oxaliplatin (FOLFIRINOX).
Five days later, she was readmitted with respiratory failure and was found to have acute segmental pulmonary embolism and worsening metastatic lung disease. Despite treatment with therapeutic heparin, her pulmonary status declined. She transitioned to hospice care six weeks after her initial diagnosis of metastatic pancreatic cancer.
DISCUSSION
According to the American Cancer Society, one-year survival for pancreatic cancer (all stages combined), is around 20%, with the five-year survival rate merely approaching 9%. Pancreatic cancer is usually asymptomatic in its early stages, and patients often present late in the course of the disease with abdominal pain, jaundice, and weight loss. There are currently no screening recommendations for pancreatic cancer in the United States.
Presentation of metastatic pancreatic adenocarcinoma with dyspnea from lymphangitic spread is uncommon. Abdominal CT scan is not routinely performed in cases of uncomplicated pancreatitis presenting with mild symptoms in a young patient with obvious inciting factor and rapid resolution of abdominal pain with conservative therapy.
Additional review of this patient’s medical record revealed that she did receive abdominal CT scan upon her initial presentation with pancreatitis, and there was a 13 mm pancreatic mass versus developing necrotizing pancreatitis and early pseudocyst reported. Unfortunately, patient was lost to short-term follow up at that time.
This scenario highlights importance of considering an early referral for lung biopsy in cases of diagnostic uncertainty. Timely diagnosis and proper therapy could offer life-prolonging and life-saving modalities in this setting.
CITATIONS
- Li, S, Tian, B. Acute pancreatitis in patients with pancreatic cancer. Medicine (Baltimore) 2017; 96(3): e5908
- Aslam, Zhi, Nadeem, Arsalan, Wallach. A case of rapidly deteriorating lymphangitic carcinomatosis in a patient with stage IV pancreatic cancer. Cureus 2019; 11(4): e4421
- Bruce DM, Heys SD, Eremin O: Lymphangitis carcinomatosa: a literature review. J R Coll Surg Edinb. 1996, 41:7-13.
- Thomas A, Lenox R. Pulmonary lymphangitic carcinomatosis as a primary manifestation of colon cancer in a young adult. CMAJ. 2008; 179(4): 338-340. doi:10.1503/cmaj.080142.


Be the first to comment on "Faculty Development Case of the Month: March 2021"